In recent years, the world has faced multiple health challenges, and Monkeypox, or Mpox, has become one of the most talked-about diseases. Although it’s a rare disease, the outbreaks in 2022 and 2023 have brought global attention to its transmission and impact. This blog delves into everything you need to know about this Monekypox disease: what it is, how it spreads, its symptoms, and who is most at risk. We will also cover vital information on prevention, treatment options, and the latest updates on Monkeypox cases in India. By staying informed and taking the right precautions, we can better protect ourselves and our communities from this emerging health threat.
What is Monkeypox?
Mpox is a rare disease caused by the monkey virus. It is a viral disease that can transfer from animals to humans. Despite its name, the monkeypox is not solely associated with monkeys; it can be found in several other animals, including squirrels and rats. It’s similar to smallpox and was first identified in 1958. However, the first human case was reported in 1970 in Central and West Africa. In recent years, there have been monkeypox virus outbreaks in other parts of the world, including Europe, the United States and Australia. This makes the disease a global concern.
Monkeypox cases in India
According to the World Health Organization, India has reported 30 cases since 2022, with the most recent case in March 2024. The first monkeypox case in India was reported in July 2022.
How Common is Monkeypox?
Monkeypox is relatively rare. Outbreaks are typically small and localised. However, in recent years, there have been larger monkeypox virus outbreaks, including a global outbreak in 2022, unlike previous outbreaks, where transmission was primarily through contact with infected animals. The recent outbreak showed sustained human-to-human transmission, especially through close physical contact, including skin-to-skin contact during intimate interactions.
How is Monkeypox Transmitted?
Mpox spreads through close contact with an infected person or animal. This can be transmitted by:
-
Direct Contact: Close physical contact with infected individuals, particularly skin lesions, bodily fluids or transmission.
-
Contaminated Objects: Sharing items like bedding, clothing or towels that have come into contact with an infected person can spread the virus.
-
Animal to Human Transmission: Contact with infected animals, such as rodents or non-human primates. This can also cause infection.
It’s important to note that the virus can be transmitted through respiratory droplets. It generally requires prolonged face-to-face contact. This makes it less contagious than diseases like COVID-19.
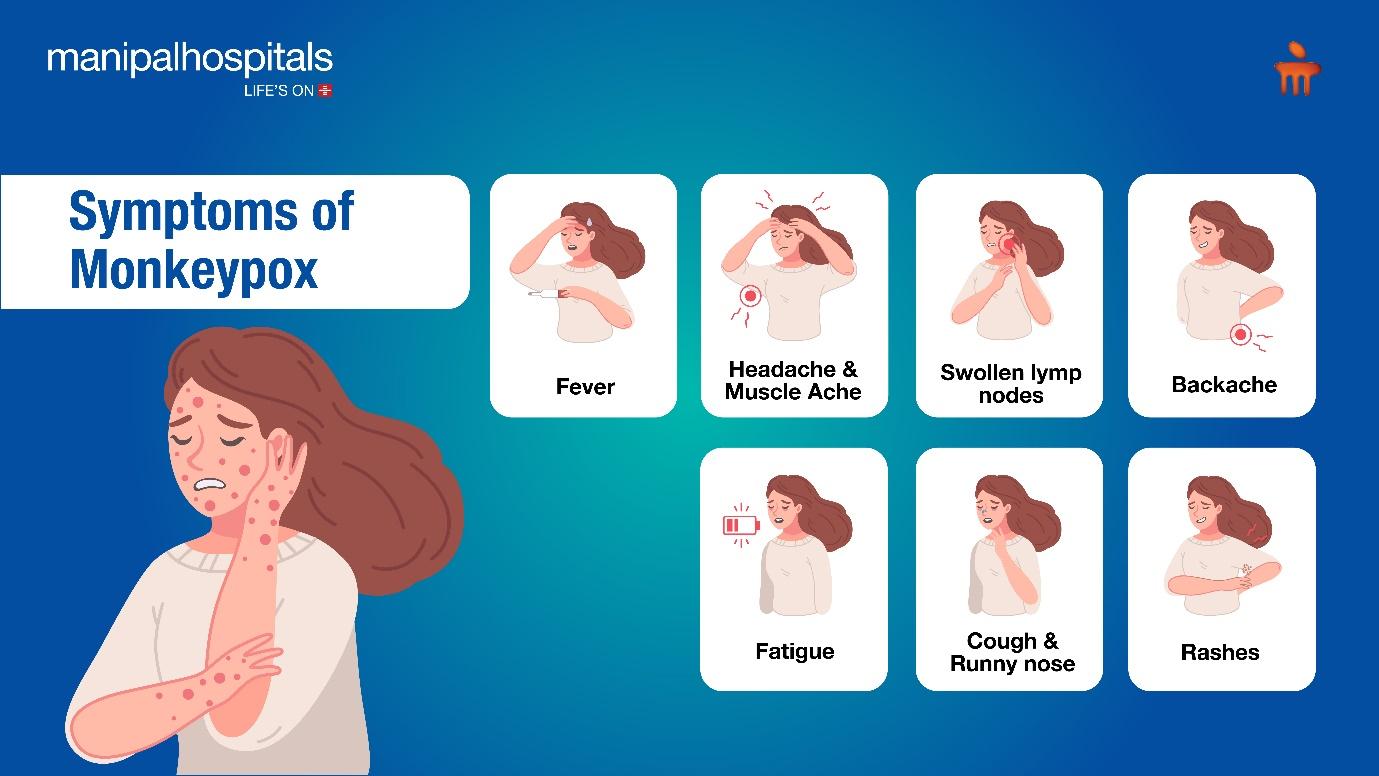
What are the Symptoms of Monkeypox?
The monkeypox virus symptoms usually appear within 1 to 3 weeks after exposure to the virus. The monkeypox symptoms may include:
-
Fever
-
Headache
-
Muscle Ache
-
Backache
-
Swollen lymph nodes
-
Fatigue
-
Cough
-
Runny nose
-
Rashes
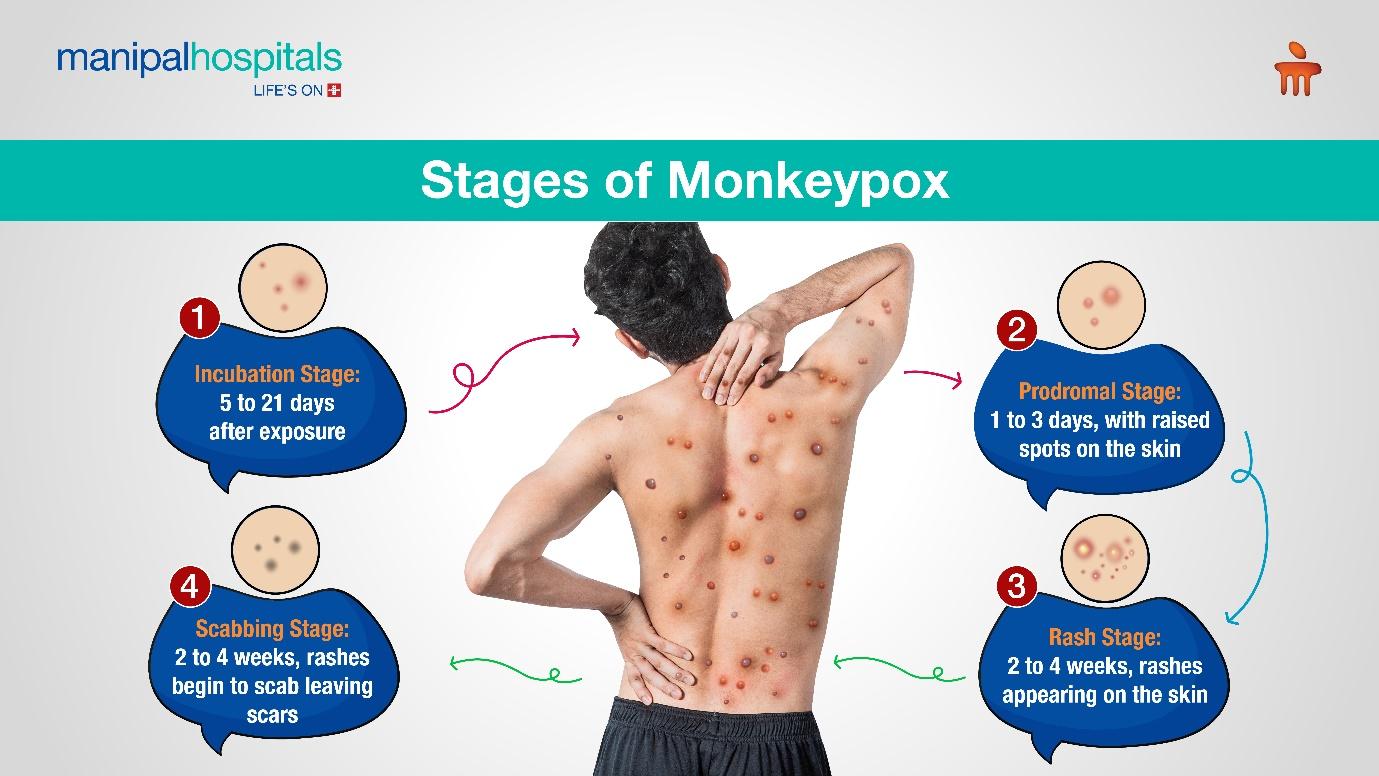
The rash is the most recognisable symptom and progresses through stages from flat lesions to pus-filled blisters.
Who is at Risk?
Although anyone can contract monkeypox, however, certain groups are more vulnerable, such as:
-
Individuals with close contact with infected persons, including household members and caregivers.
-
People with weak immunity systems.
-
Healthcare workers who are exposed to infected patients.
-
Communities with higher transmission rates. Especially where close physical contact occurs.
Is monkeypox dangerous?
Monkeypox can be dangerous for pregnant women, people with chronic diseases like HIV, newborns, children and people with low immunity. Travellers and those with multiple sexual partners are also at higher risk. Though Mpox is a self-limiting disease, it mostly resolves on its own. However, in severe cases, it can be life-threatening.
Monkeypox Treatment
As of August 2024, there isn’t a specific treatment officially approved for monkeypox (mpox). However, certain antiviral drugs may aid in managing the infection:
Tecovirimat (TPOXX):
This is the primary medication used for treating Mpox, particularly in children, adolescents, and individuals with weakened immune systems. Although TPOXX is approved by the FDA for smallpox, its effectiveness and safety for Mpox are still being studied. Currently, it can be accessed through the Study of Tecovirimat for Mpox (STOMP) clinical trial or the CDC’s expanded access (compassionate use) program.
Other Antiviral Medications:
Options like brincidofovir (Tembexa), cidofovir (Vistide), and intravenous vaccinia immune globulin (VIGIV) may also be considered in certain cases.
Most people recover from Mpox within 2 to 4 weeks without needing specific treatment. However, some may develop severe symptoms, such as eye infections, neurological issues, or complications from mucosal lesions. In these cases, antiviral treatments might be necessary.
Alongside antiviral therapy, supportive care and pain management can help patients recover more comfortably. Additionally, it’s crucial to take steps to prevent the spread of Mpox, such as informing those you’ve been in close contact with. Consult our infectious expert if you need monkeypox virus treatment.
Is Moneypox curable?
Mpox is usually a self-limited disease and gets better without treatment. The symptoms of Mpox generally last from two to four weeks. Following a diagnosis, the healthcare provider will diligently monitor the condition, effectively to alleviate the monkeypox virus symptoms, prevent dehydration, and promptly administer antibiotics to treat any secondary bacterial infections that may develop.
Here are some common approaches to cure from Mpox:
-
Supportive care
-
Smallpox Vaccine
-
Isolation and Infection Control
Monkeypox Prevention
Preventing the spread of monkeypox involves both personal and community-level actions:
-
Avoid Close Contact: Refrain from close physical contact with people who have visible rashes or symptoms.
-
Practice Good Hygiene: Regular handwashing with soap and water or using alcohol-based hand sanitisers is crucial.
-
Protective Measures: Use personal protective equipment (PPE) and follow strict infection control protocols for healthcare workers in healthcare settings.
-
Vaccination: For those at higher risk, such as healthcare workers and close contacts of confirmed cases, the MPOX vaccine is an effective form of prevention.
What Should You Do if You Suspect Monkeypox Symptoms?
If you or your loved ones suspect or have Mpox symptoms, it is advised to consult with a medical professional. You can also take some immediate action to manage the disease, they are:
-
Isolation: Avoid having any contract with others.
-
Take oatmeal baths: Taking a warm colloidal oatmeal bath can relieve the rashes.
-
Cover the rash: Over the rashes with a bandage to limit the spread to others.
-
Pain and fever reducers: Take medicines to relieve the pain and reduce the fever.
-
Take good care: Wash your hands and maintain good hygiene to manage the disease.
A new strain of Monkeypox: Clade 1b
The emergence of clade 1b, a more transmissible monkeypox variant, is causing concern. Children are particularly vulnerable to severe illness.
Health organisations worldwide are closely monitoring the spread of clade 1b monkeypox and implementing measures to contain its spread. These measures include surveillance, contact tracing, and public health campaigns to raise awareness and promote prevention.
The recent monkeypox virus outbreak serves as a reminder of the ever-present threat posed by zoonotic diseases. While the situation is concerning, awareness, vaccination, and public health measures are vital in controlling the spread. As with many diseases, monkeypox has been surrounded by stigma and misinformation. Particularly regarding its modes of transmission. It’s essential to approach the outbreak with accurate information and empathy. We should also ensure that affected individuals receive proper care without discrimination. In such cases, communities can work together to reduce the impact of the outbreak. Staying informed and practising good hygiene are crucial steps in protecting from monkeypox and other infectious diseases.