Endotracheal tubes (ET tubes) are critical tools in modern medicine, particularly in emergency and surgical settings. They facilitate airway management by ensuring a clear path for air to enter the lungs, making them indispensable for patients who are unable to breathe independently. This guide will explore what endotracheal tubes are, their various uses, preparation for insertion, and important considerations for their removal.
What is an Endotracheal Tube?
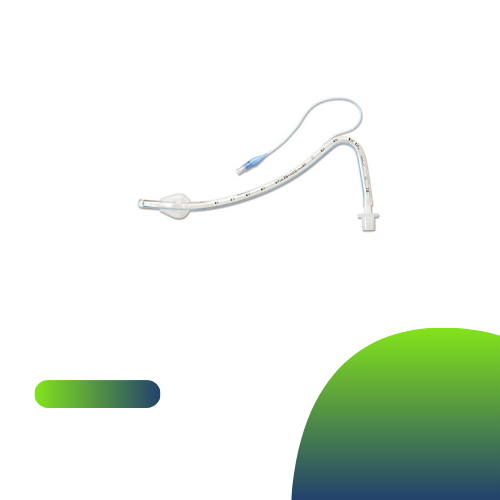
An endotracheal tube is a flexible plastic tube that is inserted into the trachea (windpipe) through the mouth or nose. It serves several functions, primarily to secure the airway during anesthesia, emergency resuscitation, or mechanical ventilation. ET tubes come in various sizes to accommodate patients of different ages and anatomies, ensuring effective airway management.
Uses of Endotracheal Tubes
Endotracheal tubes are primarily used for:
1. Airway Protection: They prevent airway obstruction, especially in unconscious patients or those with reduced protective reflexes.
2. Mechanical Ventilation: ET tubes allow for controlled breathing when a patient cannot breathe on their own, such as during surgery or severe respiratory distress.
3. Aspiration Prevention: By maintaining a secure airway, ET tubes reduce the risk of aspiration, where stomach contents enter the lungs, which can lead to pneumonia.
Why Are Endotracheal Tubes Used?
Endotracheal tubes are utilized in a variety of medical situations, including:
– Surgical Procedures: During general anesthesia, ET tubes ensure that the airway remains open and secure while the patient is unconscious.
– Emergency Situations: In cases of severe respiratory failure, trauma, or cardiac arrest, ET tubes provide immediate access to the airway, allowing for effective ventilation and oxygenation.
– Critical Care: Patients in intensive care units (ICUs) often require ET tubes for prolonged mechanical ventilation due to conditions like acute respiratory distress syndrome (ARDS) or chronic obstructive pulmonary disease (COPD).
Endotracheal Tube Types and Sizes
ET tubes are available in various sizes and designs, tailored for specific patient populations:
– Sizes: The diameter of the tube is measured in millimeters, with sizes ranging from 2.5 mm for infants to 10 mm for adults. The choice of size depends on the patient’s age, size, and clinical condition.
– Types: There are cuffed and uncuffed tubes. Cuffed tubes have an inflatable balloon that seals the airway, preventing air leaks and aspiration. Uncuffed tubes are typically used in pediatric patients to reduce the risk of airway injury.
How to Prepare for an Endotracheal Tube
Preparation for endotracheal intubation involves several crucial steps:
1. Patient Assessment: Conduct a thorough assessment, including reviewing the patient’s medical history, airway anatomy, and any potential difficulties.
2. Informed Consent: If possible, obtain consent from the patient or their family, explaining the procedure and its purpose.
3. Equipment Setup: Ensure all necessary equipment is ready, including the ET tube, laryngoscope, suction device, and bag-valve-mask (BVM) for ventilation.
Endotracheal Tube Removal
Once a patient no longer requires mechanical ventilation or airway protection, the ET tube can be safely removed:
1. Weaning Process: Assess the patient’s readiness for extubation by checking respiratory function, oxygenation, and the ability to protect the airway.
2. Procedure: Administer supplemental oxygen and ensure that emergency equipment is available. Carefully deflate the cuff of the ET tube and gently remove it while monitoring the patient’s respiratory status.
3. Post-Extubation Care: Observe the patient for any signs of respiratory distress or complications. Provide support as needed, and implement strategies to maintain airway patency.
Conclusion
Endotracheal tubes are essential tools in ensuring airway safety and effective ventilation in various medical settings. Understanding their uses, preparation for insertion, and removal procedures is crucial for healthcare professionals. Continuous training and adherence to best practices will enhance patient outcomes and minimize risks associated with endotracheal intubation. As medical technologies evolve, staying informed about advancements in airway management will further improve the safety and efficacy of using endotracheal tubes in clinical practice.